Chronic pain does not make sense under the (bio)medical model
Everyone knows that pain is what happens when your body is hurt. When you first skinned your knee on the sidewalk, you cried because our knee was damaged and you were bleeding. When you stubbed your toe on the table leg last week, it hurt because the muscles and ligaments around the toe were injured. Your body is damaged, and so you have pain.
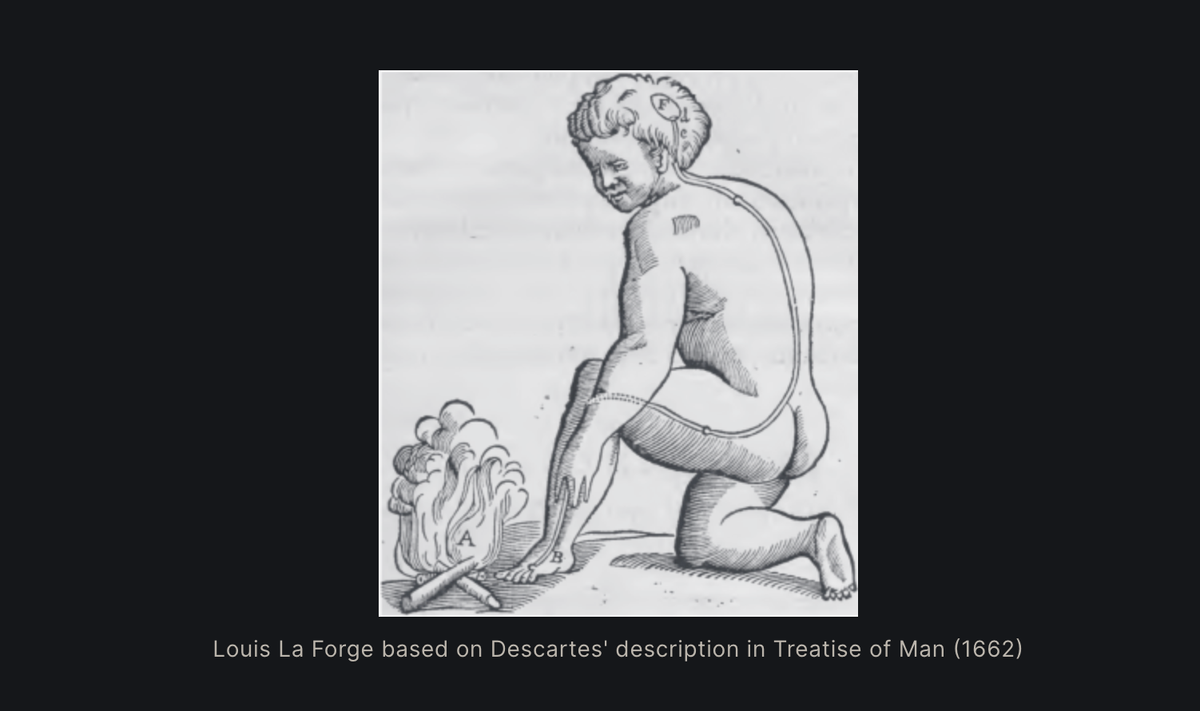
Many doctors will explain pain similarly. They say that pain is what happens when noxious stimuli cause pain receptors (‘nociceptors’) to fire, sending a signal up the spinal cord, which the brain receives as pain. In other words, pain is input to the brain from pain receptors detecting potential tissue damage.

The heat of the flame near the foot activates a pain receptor within the nerve tubule that traverses up the leg, to the spinal cord, and finally, to the brain.
This illustration captures Descartes’ theory of pain as he articulated it in the 17th century. It remains the foundation for our biomedical theory of pain, which we naturally extend to chronic pain1. The logic it articulates is as follows:
Tissue damage → Nociceptors release → Experience of pain
or
Pain = tissue damage
If your back hurts, for example, doctors can tell you what is wrong by using imaging techniques (CT, X-ray, or MRI) and either send you to physical therapy, give you painkillers, or surgically operate on you.
- CT scans, X-rays, and MRIs allow diagnosis of structural abnormalities like a herniated disc (when one rubbery disc between the spinal vertebrae ruptures) or spinal stenosis (pinching when a spinal column narrows).
- Physical therapy operates on the principle that your muscles are imbalanced, and that, to reduce your back pain, you need to improve your abdominal muscles to put less stress on the spine.
- Painkillers don’t address the cause, but help reduce pain. NSAIDs inhibit inflammation and primary nociception at the site of the pain. Opioids bind receptors in the brain and central nervous system and reduce the response to pain.
Under this model, pain is more or less passively received from the environment. And the two ways we can address pain are either by i) helping fix tissue damage in the body, ii) reducing the firing of the pain pathways.
It was only later that I understood that
this model of pain is subtly, dangerously wrong.
A few observations to motivate skepticism about this default biochemical theory of pain:
1. Many people have major “structural musculoskeletal damage” without pain.
In a widely cited 1994 study, MC Jensen et al. examined the MRI images of the backs of 98 pain-free people. Of the participants, aged twenty and older, over half had an abnormality in at least one disk2. Herniation or disk bulges were strikingly common in patients who were pain free. There are many other studies demonstrating the frequency of the “spinal abnormalities” that are often used to explain back pain3.
Studies have demonstrated similar findings for labral tears in hips, scarred rotator cuffs, knees without cartilage. Repeatedly we have seen those with major structural musculoskeletal damage be entirely pain free.
This demonstrates two things. First, that it is possible and indeed likely very common for there to be structural damage without pain. Second, that common imaging techniques should not be heavily relied upon for diagnosis.
2. In general, we often experience tissue damage without pain
All of us at some point have experienced tissue damage without pain. For athletes, it’s a familiar experience to wake up with a bruise or scratch with no clear recollection of how it got there. We have surely all woken up noticing the next day after a tough hike in the woods, a hard workout, or some other intense physical activity, and been surprised at the pain in our body that wasn’t there the day before.
Anecdotes from war can illustrate more extreme cases of tissue damage without pain. Henry Beecher, an anesthesiologist on the battlefield of the Anzio Beachhead in Italy during WWII, found an astounding lack of reported pain among severely wounded soldiers4. He surveyed the reported pain intensity of 215 lucid men that had penetrating wounds in the head, chest, or stomach, compound bone fractures, or extensive soft-tissue wounds. Three-quarters of the soldiers with severe wounds had so little pain that they refused pain relief medication.
3. We also have pain without tissue damage
Phantom limb pain
People who have had limbs amputated often report intense pain in the absent limb. The pain is usually intermittent, and is often vividly described as throbbing, stabbing or burning. Researchers have been able to distinguish between pain at the stump, and pain within the missing limb itself. In this case, there is no tissue damage in the absent limb, yet there are recurring episodes of pain long after the wound has healed.
Nonspecific lower back pain
Hundreds of millions of adults experience ongoing nonspecific lower back pain5. ‘Nonspecific back pain’ is what doctors will call reports of pain when the CT/MRI/X-rays reveal a structurally healthy spine, and other pathologies (infections, tumors, osteoporosis, etc) have also been ruled out. In other words, a large fraction of the world’s population experiences pain that cannot be linked to tissue damage.
Emotional pain
Many of the most painful experiences that we undergo have no underlying tissue damage. Remember the heartbreak after your first love, or the grief and newfound loneliness at the death of a dear family member. Even though our ‘heart is broken’, there is no underlying cardiovascular damage. Similarly, although ‘our stomach sinks’ in response to grief, it remains structurally sound.

How does the biochemical model account for emotional pain? Mostly, it doesn’t have a response, and cannot acknowledge the reality of pain from non-structural factors. Under the biochemical model of pain, emotional pain is ‘in the head’ and consequently considered ‘less real’ than physical pain.
Some other observations that don’t make sense under the standard model of pain:
- People older than 60 generally experience less back pain that those younger than 60
- Distraction helps you cope with pain
- Depressed and anxious people are more likely to experience chronic pain.
Like this essay? Sign up for my newsletter here.
In the next post, I'll outline a theory of pain that can can address some of these mysteries.
- Note that for chronic pain, I’m mostly referring to relatively generalized (non-localized) syndromes. Examples include low back pain, migraine headaches, tendinitis, repetitive stress injury, carpal tunnel, fibromyalgia, chronic fatigue syndrome. For reference, 85% of reported back pain in the U.S. is nonspecific and falls into this category. Non-examples: ongoing lesions on body, pain from identified cancerous tumors.
- Jensen, Maureen C., et al. "Magnetic resonance imaging of the lumbar spine in people without back pain." New England Journal of Medicine 331.2 (1994): 69-73.
- Weinreb JC, Wolbarsht LB, Cohen JM, Brown CEL, Maravilla KR. Prevalence of lumbosacral intervertebral disk abnormalities on MR images in pregnant and asymptomatic nonpregnant women. Radiology 1989;170:125-128; Hitselberger WE, Witten RM. Abnormal myelograms in asymptomatic patients. J Neurosurg 1968;28:204-206
- Beecher, Henry K. "Pain in men wounded in battle." Annals of surgery 123.1 (1946): 96.
- The WHO estimates that that around 620 million people experience lower back pain worldwide; GBD 2021 Low Back Pain Collaborators. Global, regional, and national burden of low back pain, 1990-2020, its attributable risk factors, and projections to 2050: a systematic analysis of the Global Burden of Disease Study 2021. Lancet Rheumatol 2023: 5: e316-29